Lung Cancer Answers is a website devoted to life issues for lung cancer patients and their families and is sponsored by Brad Cooper* of Cooper, Hart, Leggiero & Whitehead, PLLC. Cooper, Hart, Leggiero & Whitehead is located in The Woodlands, Texas (Greater Houston Area), handles cases nationwide with co-counsel in state of filing, and can be reached toll-free at 1-800-998-9729 for more information on lung cancer. Brad Cooper is not a medical doctor. The information on these pages is for the education of lung cancer patients and their families regarding potential medical and legal options. Patients are advised to consult with a medical doctor.
* Licensed by the Supreme Courts of Texas.
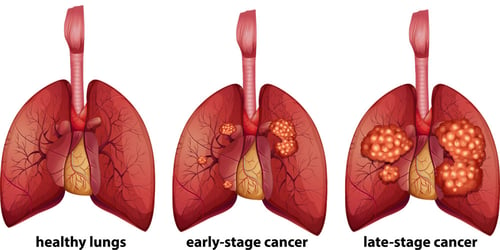
Staging of Lung Cancer
Staging is the process used to learn how much cancer is within the body and if it has spread. As with most cancers, staging is an essential part of determining how severe the patient’s lung cancer is and the best treatment plan.
Staging Non-Small Cell Lung Cancer
The stage of Non-Small Cell Lung Cancer (NSCLC) is determined based on various factors, including:
- The size and location of the tumor
- If the lung cancer has spread to the lymph nodes or other areas of the body
Each stage of non-small cell lung cancer are determined based on the traits outlined below:
Stage: Occult (hidden cancer)
The tumor is found only in the lining of the airways. It has not spread to other parts of the body.
Stage: 0
In stage 0 lung cancer, abnormal cells are found in the airway lining. Abnormal cells can become cancerous and spread into normal, nearby tissue. Stage 0 may be squamous cell carcinoma in situ (SCIS) or adenocarcinoma in situ (AIS).
Stage 1
Stage: IA
In stage IA lung cancer, the tumor is less than or equal to 3 centimeters and is contained to the lung (not having spread to any lymph nodes). Stage IA tumors may be further divided into IA1, IA2, or IA3 based on the tumor’s size.
Stage: IB
The lung cancer tumor is greater than 3 centimeters but not larger than 4 centimeters and is contained in the lungs (has not spread to the lymph nodes).
OR
The tumor is 4 centimeters or smaller with one (or more) of the following:
- Cancer has spread to the deepest layer of the membrane that covers the lung.
- Cancer has spread to the primary bronchus but not to the carina.
- Part (or all) of the lung has collapsed or has developed pneumonitis.
Cancer has not spread to the lymph nodes.
Stage 2
Stage: IIA
The lung cancer tumor is between 4 - 5 centimeters, contained in the lung (has not spread to the lymph nodes), and has one or more of the following:
- Cancer has spread to the primary bronchus but has not spread to the carina.
- Cancer has spread to the deepest layer of the membrane that covers the lung.
- All or part of the lung has collapsed or has developed pneumonitis.
Stage: IIB
The tumor is less than 5 centimeters and has spread to the lymph nodes on the same side of the chest as the primary tumor. The cancerous lymph nodes are in the lung or near the bronchus. Also, one (or more) of the following may be found:
- Cancer has spread to the main bronchus but has not spread to the carina.
- Cancer has spread to the innermost layer of the membrane that covers the lung.
- Part of the lung or the whole lung has collapsed or has developed pneumonitis.
OR
Cancer has not spread to the lymph nodes, and one (or more) of the following is found:
- The tumor is larger than 5 but less than 7 centimeters.
- There are different tumors (one or more) in the same lobe of the lung as the primary tumor.
- Cancer has spread to any of the following:
- Chest wall
- The membrane that lines the inside of the chest wall
- The nerve that controls the diaphragm
- The outer layer of tissue of the sac around the heart
Stage 3
Stage: IIIA
The tumor is 5 centimeters or less, and the lung cancer has spread to lymph nodes on the same side of the chest as the primary tumor. The cancerous lymph nodes are found around the trachea or aorta or where the trachea splits into the bronchi. Additionally, one or more of the following may be found:
- Cancer has spread to the main bronchus but has not spread to the carina.
- Cancer has spread to the deepest layer of the membrane that covers the lung.
- Part of the lung or the whole lung has collapsed or has developed pneumonitis.
OR
Cancer has spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are in the lung or near the bronchus. Also, one or more of the following:
- The tumor is larger than 5 but less than 7 centimeters. There are one or more separate tumors in the same lobe of the lung as the primary tumor.
- Cancer has spread to any of the following areas:
- The chest wall or the membrane that lines the inside of the chest wall.
- The nerve that controls the diaphragm.
- The outermost layer of tissue of the sac around the heart.
OR
Lung Cancer may have spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are in the lung or near the bronchus. Also, one or more of the following:
- The tumor is bigger than 7 centimeters.
- There are one or more separate tumors in a different lobe of the lung, with the primary tumor.
- The tumor is any size, and cancer has spread to any of the following:
- Aorta or vena cava - the major blood vessels that lead to or from the heart
- Breastbone or backbone
- Carina
- Diaphragm
- Esophagus
- Heart
- Trachea
- Voicebox - the nerve that controls the larynx
Stage: IIIB
The tumor is 5 centimeters or less and has spread to the lymph nodes above the collarbone on the same side of the chest as the primary tumor or to any lymph nodes on the opposite side of the chest as the primary tumor. Also, one or more of the following may be found:
- Cancer has spread to the main bronchus but has not spread to the carina.
- Cancer has spread to the innermost layer of the membrane that covers the lung.
- Part of the lung or the whole lung has collapsed or has developed pneumonitis.
OR
The tumor may be any size, and cancer has spread to lymph nodes on the same side of the chest as the primary tumor. The lymph nodes with cancer are around the trachea or aorta, or where the trachea divides into the bronchi. Also, one or more of the following:
- There are one or more separate tumors in the same lobe or a different lobe of the lung with the primary tumor.
- Cancer has spread to any of the following:
- The membrane that lines the inside of the chest wall
- Chest wall
- The nerve that controls the diaphragm
- The outermost layer of tissue of the sac around the heart
- Trachea
- Carina
- Esophagus
- Breastbone or backbone
- Diaphragm
- Heart
- aorta or vena cava - the major blood vessels that lead to or from the heart
- Voicebox- the nerve that controls the larynx
Stage: IIIC
The tumor may be any size, and cancer has spread to lymph nodes above the collarbone on the same side of the chest as the primary tumor or to any lymph nodes on the opposite side of the chest as the primary tumor. Also, one or more of the following:
- There are one or more separate tumors in the same lobe or a different lobe of the lung with the primary tumor.
- Cancer has spread to any of the following:
- Aorta or vena cava - the major blood vessels that lead to or from the heart
- The chest wall or the membrane that lines the chest wall
- The nerve that controls the diaphragm
- The outermost layer of tissue of the sac around the heart
- Trachea
- Carina
- Esophagus
- Breastbone or backbone
- Diaphragm
- Heart
- Voicebox - the nerve that controls the larynx
Stage 4
Stage: IVA
An IVA tumor may be any size. The lung cancer may have spread to the nearby lymph nodes, and one (or more) of the following:
- There are tumor(s) in the lung that does not have the primary tumor.
- Cancer is present in the lining around the lungs or the sac around the heart.
- Cancer is present in the fluid around the lungs or heart.
- Cancer has spread to an organ that is not near the lungs, such as the brain, adrenal gland, kidney, liver, bone, or to a lymph node that is not near the lungs.
Stage: IVB
The lung cancer has spread to multiple places in one or more organs that are not near the lung.
Treatment of Non-Small Cell Lung Cancer
Standard treatment options for NSCLC include surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. However, there are always cancer researchers studying newer and more advanced options for treating NSCLC. Some patients may require a combination of treatments.
Staging Small Cell Lung Cancer
 Other tests and procedures that may be used in the staging process for small cell lung cancer (SCLC) can include the following:
Other tests and procedures that may be used in the staging process for small cell lung cancer (SCLC) can include the following:
- Blood and urine tests
- Imaging tests (X-ray, CT, MRI)
- Endoscopic ultrasound (EUS)
- Lymph node biopsy
- Radionuclide bone scan
- Bone marrow aspiration and biopsy
Stages of Small Cell Lung Cancer
Small cell lung cancer (SCLC) falls under one of two categories, limited and extensive.
- Limited: Limited stage means that the cancer is only in one part of the chest, and radiation therapy could be a treatment option. About one out of three people with SCLC have limited stage disease when first diagnosed.
- Extensive: Extensive stage describes SCLC that has spread to the opposite lung or distant sites in the body such as the brain, bone, or bone marrow. This term is also sometimes used to describe SCLC that has spread to the fluid around the lung. About two out of three people with SCLC have an extensive disease when their lung cancer is found.
Treatment of SCLC
Treatment of lung cancer is based mostly on whether the cancer stage is limited or extensive. Your medical oncologist may decide to treat your SCLC in various ways, such as:
- surgery
- radiation therapy
- chemotherapy
- laser therapy
- immunotherapy
- endoscopic stent placement

©2024 Cooper, Hart, Leggiero & Whitehead, PLLC. All rights reserved.